Shock Loss After Hair Transplant: Why It Happens
Shock loss after hair transplantation is a common, temporary shedding phase caused by surgical trauma, inflammation, and hair-cycle shifts. Read why it happens, who is most at risk, how donor and recipient areas are affected.
Why It Happens and What to Expect
Hair transplantation is often seen as the final step in restoring a fuller head of hair, but many patients experience a worrying phase shortly after surgery: shock loss. Understanding why this happens, and how common can help both surgeons counsel their patients better and patients navigate the early postoperative period with more confidence.
What Is “Shock Loss”?
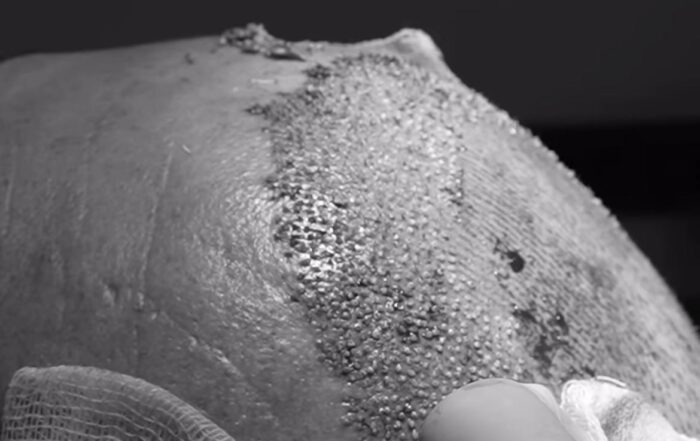
Shock loss refers to a temporary shedding of hair in the weeks following a hair transplant. It can involve both newly transplanted grafts and existing (native) hairs, and it can occur in the recipient area (where grafts were implanted) or even the donor zone. Shedding does not necessarily mean graft failure, and the roots typically remain alive.
Why Does Shock Loss Happen? Mechanisms and Risk Factors
Several factors contribute to shock loss. Understanding them can help both surgeons and patients anticipate and manage the phenomenon.
- Surgical Trauma
Even with minimally invasive techniques (e.g., FUE), the process of creating micro-incisions, inserting grafts, and operating the scalp causes mechanical stress. This trauma can prepare hair follicles to prematurely enter the telogen (resting) phase, leading to shedding. - Inflammatory Response & Vascular Disruption
The body’s natural healing response involves inflammation, which may impair blood supply to adjacent native follicles. Reduced perfusion can push hairs into shedding. - Effluvium in Donor Area (“Donor Shock Loss”)
Shock loss is not limited to the recipient site. In some cases, hairs around the donor extraction zone suffer acute effluvium, likely due to trauma and compromised blood supply after FUE harvesting. - Hair Cycle Dynamics: Telogen vs. Anagen Effluvium
- The more common form is telogen effluvium, where follicles shift into the resting phase.
- In some cases, anagen effluvium (loss of growing-phase hairs) has been described, particularly in donor sites after harvesting.
- These shifts depend on many variables, including the resilience of the follicle, ischemia during surgery, and individual patient biology.
- Patient Risk Factors
A recent retrospective study of 621 patients undergoing FUE (follicular unit excision) identified sex as a major risk factor: women had significantly higher odds of shock loss than men. Additionally, age among female patients (especially over 40) was correlated with risk. - Technical / Surgical Factors
- Poor technique, aggressive handling, or suboptimal surgical planning may magnify trauma.
- Patient selection matters: for example, in patients with many miniaturized (“weak”) native hairs, the stress of surgery may more easily push those follicles to shed.
Is Shock Loss Permanent?
In the vast majority of cases, no:
- Studies show that most shed hairs, both native and transplanted, recover: the follicles survive and re-enter the growth cycle.
- In donor area acute effluvium after FUE, recovery is often complete within weeks to months.
- However, surgeons should counsel patients that risk is not zero.
When to Be Concerned
While shock loss is generally benign and self-limiting, there are further features to evaluate:
- Shedding continues beyond 3–4 months without signs of regrowth.
- Uneven or patchy balding persists, suggesting possible graft failure or necrosis. However, recipient-site necrosis is a rare.
- In the donor area, if non-healing patches or scarring develop, further trichoscopic or histologic evaluation may be needed.
Final Point
Shock loss is a natural, common, and generally temporary phenomenon after hair transplantation. It reflects the scalp’s response to surgical trauma rather than graft death. Patient counseling, refined surgical technique, and informed follow-up are key to minimizing both the physical effects and the emotional distress for patients.
References
- Kerure AS, Agrawal SM, Dhurat R, Ginzburg A. Donor Area Acute Effluvium following Follicular Unit Extraction-Trichoscopic Simulator of Alopecia Areata: Series of Four Cases. J Cutan Aesthet Surg. 2020;13(1):31-34. doi:10.4103/JCAS.JCAS_77_19
- Loh SH, Lew BL, Sim WY. Localized Telogen Effluvium Following Hair Transplantation. Ann Dermatol. 2018;30(2):214-217. doi:10.5021/ad.2018.30.2.214
- Okochi H, Onda M, Momosawa A, Okochi M. An Analysis of Risk Factors of Recipient Site Temporary Effluvium After Follicular Unit Excision: A Single-
- Williams KL Jr, El-Maghraby S. Complications with Follicular Unit Excision. Facial Plast Surg. 2024;40(2):234-244. doi:10.1055/a-2201-8302Center Retrospective Study. Aesthetic Plast Surg. 2024;48(7):1258-1263. doi:10.1007/s00266-023-03699-z
References
- Kerure AS, Agrawal SM, Dhurat R, Ginzburg A. Donor Area Acute Effluvium following Follicular Unit Extraction-Trichoscopic Simulator of Alopecia Areata: Series of Four Cases. J Cutan Aesthet Surg. 2020;13(1):31-34. doi:10.4103/JCAS.JCAS_77_19
- Loh SH, Lew BL, Sim WY. Localized Telogen Effluvium Following Hair Transplantation. Ann Dermatol. 2018;30(2):214-217. doi:10.5021/ad.2018.30.2.214
- Okochi H, Onda M, Momosawa A, Okochi M. An Analysis of Risk Factors of Recipient Site Temporary Effluvium After Follicular Unit Excision: A Single-
- Williams KL Jr, El-Maghraby S. Complications with Follicular Unit Excision. Facial Plast Surg. 2024;40(2):234-244. doi:10.1055/a-2201-8302Center Retrospective Study. Aesthetic Plast Surg. 2024;48(7):1258-1263. doi:10.1007/s00266-023-03699-z